Alpha Gal Allergy
The Centers for Disease Control and Prevention has warned that alpha-gal syndrome is an emerging public health concern. More than 90,000 suspected cases have been documented between 2017 and 2022, yet 40% of physicians are unaware of this syndrome. The number of new cases has been increasing by approximately 15,000 each year.
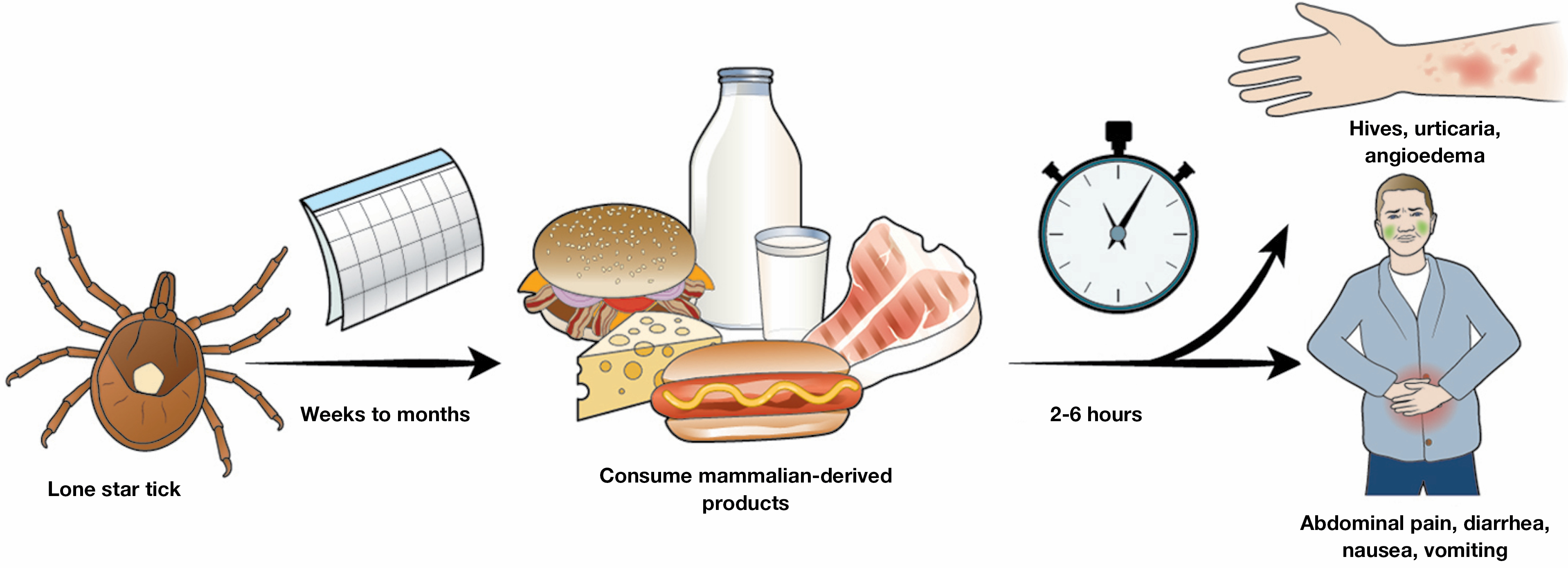
Alpha-gal (galactose-α-1,3-galactose) is a sugar molecule present in most non-primate mammals but not in fish, reptiles, birds, or people. Patients appear to be sensitized through the bites of Lone Star tick, Amblyomma Americanum, whose host is deer. Most cases have occurred in Arkansas, Kentucky, Missouri, and Suffolk County, New York.
When a sensitized human eats mammalian meat or mammalian-derived products, alpha-gal is absorbed by the GI tract bound to glycolipid, and incorporated into chylomicrons, which enter the circulation in approximately 2 hours.
When alpha-gal binds to IgE antibodies present on mast cells in the GI tract, the mast cells degranulate and release histamine and other immune mediators. They bind to sensory nerve endings causing abdominal pain, intestinal smooth muscles contractions, and mucous gland secretion.
Alpha-gal syndrome typically occurs 2 to 6 hours after a person eats beef, pork, other mammalian meat, or other food products made from mammals. Symptoms include abdominal pain, diarrhea, nausea and vomiting.
While the most common presentation is a delayed allergy to meat, anaphylaxis to alpha-gal has been reported after routine childhood vaccinations, possibly due to gelatin and/or calf serum in the vaccines. Other products, including colloid solutions, gelatins, bovine or porcine heart valves, and possibly some hemostatic agents, have also been implicated.
Diagnosis of the alpha-gal syndrome can be confirmed by testing for IgE antibodies to alpha-gal. Patient who test positive for IgE antibodies to alpha-gal should be instructed to adopt an alpha-gal avoidance diet that eliminates beef, pork, venison and related products such as lard, dairy, and ice cream. If patients are able to avoid tick bites, it may be reasonable to repeat alpha-gal IgE levels 6 to 12 months after diagnosis. As the IgE level decreases or becomes negative, patients may be able to resume eating dairy, and then mammalian meat products.
References
Stone CA, et al. Anaphylaxis after vaccination in a pediatric patient: further implicating alpha-gal allergy. J Allergy Clin Immunol Pract 2019; 7:322
McGill SK et al. AGA Clinical Practice Update on Alpha-Gal Syndrome for the GI Clinician: Commentary. Clin Gastroenterol Hepatol. April 2023, 21 (4) 891-896.
McGill SK, et al. AGA Clinical Practice Update on Alpha-Gal Syndrome for the GI Clinician: Commentary, Clin Gastroenterol Hepatol, 2023, 21:891-896.
Thompson JM, et al. Suspected Alpha-gal Syndrome Cases-United States, January 2017-December 2022. MMWR Morb Mortal Wkly Rep 2023;72:815-20.

