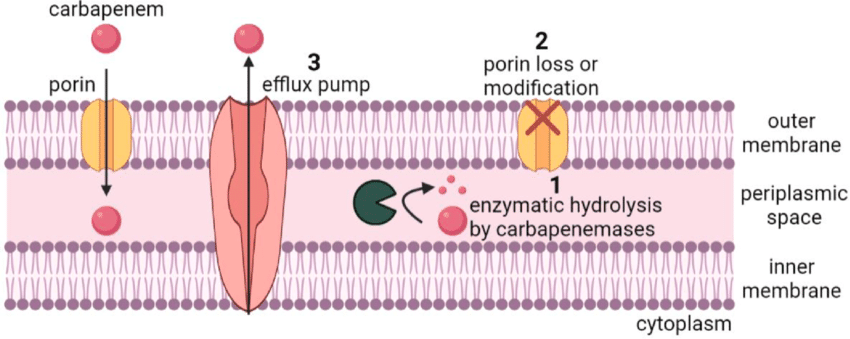
The Enterobacteriaceae are a large family of gram-negative bacilli that includes Escherichia coli, Klebsiella species, and Enterobacter species. They are normal inhabitants of the gastrointestinal tract of humans and animals and a common cause of community-acquired and health-care–acquired infections. They have gradually developed resistance to broad spectrum antibiotics. In the United States, these resistant strains have been treated with carbapenem antibiotics including imipenem, meropenem, doripenem, and ertapenem. However, new classes of enzymes that hydrolyze and inactivate the carbapenems are being detected in the United States. These carbapenemases are usually plasmid-mediated, which facilitates transfer between bacteria.
Carbapenem-resistant Enterobacteriaceae (CRE) were uncommon in the United States before 2000, but have increased in hospitals over the past 16 years. Invasive bloodstream infections with CRE have mortality rates as high as 50%. Therefore, they have become a serious infection control concern.
On September 23, 2025, the Centers for Disease Control and Prevention's (CDC's) Antimicrobial Resistance (AR) Laboratory Network reported that the incidence of carbapenemase-producing carbapenem-resistant Enterobacterales (CRE) in the United States had risen by 69% from 2019 through 2023. In addition, the incidence of CRE that produce the enzyme, New Delhi metallo-β-lactamase (NDM), has increased 460%. NDM makes CRE resistant to most antibiotics.
In 2020 alone, CRE caused about 12,700 infections and 1,100 deaths in the U.S. The infections included pneumonia, bloodstream infections, urinary tract infections and wound infections.
The most common carpabenemase is found in Klebsiella pneumoniae, and is referred to as KPC. This carbapenemase is plasmid-mediated, which facilitates transfer between bacteria. Other enteric bacteria in which this type of plamid mediated carbapenemase has been reported include E. coli, K. oxytoca, S. marcescens, E. cloacae, E. aerogenes, C. freundii, and Salmonella. Klebsiella pneumoniae carbapenemase (KPC) is encoded by a highly transmissible gene that has now spread widely throughout the United States and around the world.
In addition to KPC, other carbapenemases have emerged among Enterobacteriaceae.The best known example is NDM. NDM-producing strains are particularly problematic because they are resistant to some of the newer antibiotics that have been developed in recent years to treat carbapenem-resistant infections, leaving even fewer treatment options.
Other mechanisms besides carbapenemase enzymes that may render Enterobacteriaceae resistant to carbapenems have also been recognized. An example is AmpC beta-lactamase, which in combination with porin mutations of the bacterial cell membrane, increases antiiotic resistance.
Due to recognition of multiple types of carbapenem resistance, the CDC recently revised its definition of CRE to include any Enterobacteriaceae that is resistant to imipenem, doripenem, meropenem, or ertapenem OR is found to produce a carbapenemase.
Centers for Disease Control (CDC) & Clinical Laboratory Standards Insitute (CLSI) have issued recommendations for the detection of carpabenemases. Some gram-negative organisms producing this enzyme may fall within the susceptible range for carbapenems by automated test systems, but will exhibit an elevated MIC to carbapenems. When these organisms are also resistant to a 3rd-generation cephalosporin, such as ceftriaxone, additional testing for carbapenemase production should be performed. This confirmatory testing is called the Modified Hodge Test. Organisms tested by this method are reported as positive or negative for carbapenemase production. All carbapenems will be reported as resistant when an organism tests positive.
Current CRE prevention strategies are based on the identification of patients colonized or infected with CRE. Contact precautions are implemented for those patients harboring CRE.
Reference
Rankin DA et al. Changes in Carbapenemase-Producing Carbapenem-Resistant Enterobacterales, 2019 to 2023, Ann Intern Med; Sep 23, 2025, https://doi.org/10.7326/ANNALS-25-02404



 How to resolve AdBlock issue?
How to resolve AdBlock issue?